Clinical Insights: Respiratory Care Digital Innovation Opportunities
Co-authored by Dr Bipin Patel, CEO, electronRx, Cambridge, UK and Dr Hiromichi Yamaguchi, Yamaguchi Respiratory Clinic and Dermatology, Tokyo, Japan
August 12th, 2025
We bring together key clinical insights from respiratory specialists highlighting current gaps in asthma and COPD management, emerging technologies, and opportunities for enhanced patient care. These insights may inform strategic planning for therapeutic development and evidence generation initiatives. The findings presented herein reflect genuine clinical perspectives on unmet needs in respiratory medicine and potential areas where innovative approaches could enhance patient outcomes and prescriber confidence.
Current Clinical Evidence Gaps in Respiratory Care
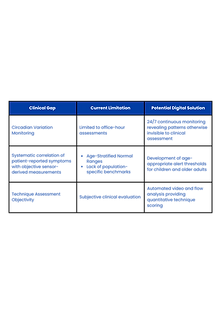
Leading respiratory specialists have identified several critical evidence gaps that currently limit optimal therapeutic decision-making:
Real-World Exacerbation Data: Clinicians require robust comparative data on annual rates of severe exacerbations across different therapeutic regimens, including accident and emergency visits, oral corticosteroid requirements, and hospital admissions. Current clinical trial data, whilst valuable, does not adequately reflect the complexity of real-world patient management scenarios.
Long-Term Safety and Tolerability Profiles: There is significant clinical demand for observational safety data spanning 6-12 months, particularly addressing concerns around pneumonia risk, eosinophilia, cardiovascular events, and other potential long-term complications. This is especially relevant for diverse patient populations, including specific ethnic cohorts where genetic and environmental factors may influence treatment response.
Patient-Reported Outcome Integration: Clinicians seek comprehensive data linking traditional clinical measures with patient-reported outcomes including Asthma Control Test scores, St George's Respiratory Questionnaire results, sleep quality assessments, and daily vitality metrics. The potential integration with wearable technology data represents an emerging area of clinical interest.
Inhaler Technique Correlation Analysis: A significant unmet need exists for quantitative assessment of inhaler technique and its direct correlation with clinical outcomes. Current subjective assessments lack the precision required for evidence-based technique optimisation and outcome prediction.
Barriers to Optimal Patient Participation
Clinical experience suggests several innovative approaches could enhance patient engagement with respiratory care:
Enhanced Monitoring Experiences: The concept of "taster sessions" utilising continuous respiratory monitoring could significantly improve patient motivation for ongoing care participation. Visual representation of breathing patterns and physiological data could create powerful patient engagement opportunities.
Streamlined Clinical Workflows: Pre-visit data collection including peak flow measurements, breathlessness scores, and respiratory rate monitoring could optimise consultation efficiency whilst improving clinical assessment quality. Digital platforms enabling secure data upload prior to appointments represent a significant workflow enhancement opportunity.
Continuous Care Connectivity: Push notification systems for medication reminders and follow-up scheduling could address the challenge of patient non-attendance and treatment non-adherence. Educational content delivery through always-accessible digital platforms may enhance patient understanding and self-management capabilities.

Clinical Knowledge Gaps in Respiratory Disease Management
Several critical knowledge gaps limit optimal care for respiratory patients, especially those newly diagnosed:
Pre-Exacerbation Physiological Signatures: Current clinical practice lacks validated biomarkers for early exacerbation detection. Time-series analysis of respiratory rate, tidal volume, and cough frequency patterns could potentially identify predictive signatures 7-14 days before clinical deterioration, enabling proactive intervention strategies.
Adherence and Persistence Determinants: The complex interactions between lifestyle factors, environmental exposures, psychological stress, and treatment persistence remain poorly understood. Digital monitoring technologies may provide unprecedented insights into real-world adherence patterns and their clinical correlates.
Digital Biomarker Validation: Emerging technologies enabling analysis of respiratory sounds, activity patterns, and physiological parameters require clinical validation to determine their predictive accuracy for disease progression and treatment response. This represents a significant research opportunity with potential clinical applications.
Behavioural Intervention Optimisation: The effectiveness of various digital engagement strategies, including notifications, gamification elements, and personalised feedback mechanisms in sustaining long-term self-management behaviours requires systematic evaluation.
Real-Time Technique Optimisation: AI-powered video and flow analysis systems could provide immediate inhaler technique feedback, coaching patients on optimal inhalation speed, breath-hold duration, and other critical technique elements. This represents a potentially transformative advancement in patient education and treatment optimisation.
Proactive Clinical Response Systems: Automated alert systems detecting sustained abnormal physiological trends could enable rapid clinical response, potentially preventing exacerbations through timely intervention. Integration with clinical workflows and multidisciplinary care teams could significantly enhance care coordination.
Personalised Self-Management Programmes: Digital platforms offering customised respiratory rehabilitation content, environmental optimisation guidance, and tailored action plans could empower patients whilst reducing clinical workload. The integration of these systems with clinical oversight represents an emerging care model of significant interest.
Critical Real-World Evidence Opportunities
Several specific clinical knowledge gaps represent significant research and development opportunities:
Market Expansion and Patient Identification Opportunities
Clinical experts suggest several approaches for broader patient identification and risk assessment:
Integrated Risk Assessment Tools: Development of risk scoring algorithms incorporating smoking history, occupational exposures, chronic cough patterns, and age demographics could facilitate systematic identification of high-risk individuals requiring clinical evaluation.
Cross Specialty Screening Protocols: Implementation of screening programmes within pharmacy settings and non-respiratory clinical specialties could identify patients with unrecognised respiratory disease. This approach could be particularly valuable for elderly patients and those with multiple comorbidities.
Community Based Monitoring Initiatives: Integration of respiratory monitoring capabilities within community health programmes, district nursing services, and primary care settings could enable population-level health assessment and early disease detection.
Public Awareness and Screening Campaigns: Respiratory health assessment initiatives offering short-term monitoring experiences could identify high-risk individuals whilst raising public awareness of respiratory disease symptoms and management options.
Clinical Evidence Priorities for Therapeutic Development
Clinical specialists have identified several high-priority evidence generation areas:
Comparative Effectiveness Research: Real-world comparative effectiveness studies examining different therapeutic approaches across diverse patient populations could provide crucial evidence for clinical decision-making and guideline development.
Long-Term Adherence and Persistence Studies: Systematic analysis of 6-12 month treatment persistence patterns and their determinants could inform both therapeutic development and patient support programme design.
Expanded Patient-Reported Outcome Assessment: Integration of sleep efficiency metrics, physical activity measurements, and quality of life trajectories with traditional clinical outcomes could provide comprehensive treatment effect assessment.
Digital Biomarker Clinical Validation: Rigorous validation of digital monitoring technologies against established clinical assessment methods could establish new standards for remote patient monitoring and care optimisation.

Strategic Considerations for Clinical Innovation
The respiratory care landscape presents several opportunities for clinical innovation leadership:
Guideline Development Influence: Generation of high-quality real-world evidence could significantly influence clinical practice guidelines and treatment algorithms, establishing new standards of care whilst supporting therapeutic positioning.
Key Opinion Leader Engagement: Collaborative research initiatives with leading respiratory specialists could enhance clinical education efforts whilst generating peer-reviewed publications in premier medical journals.
Healthcare Provider Education: Development of comprehensive educational programmes addressing digital health integration, optimal therapeutic selection, and patient management protocols could enhance prescriber confidence and appropriate therapeutic utilisation.
Integrated Care Pathway Development: Creation of evidence-based care pathways incorporating digital monitoring, therapeutic optimisation, and patient support services could establish new benchmarks for respiratory care delivery.
Strategic Implications for Consideration
In conclusion these clinical insights reveal significant opportunities for innovation in respiratory care delivery and therapeutic development. The convergence of clinical needs, technological capabilities, and regulatory acceptance of real-world evidence creates a unique environment for strategic initiative development. The clinical insights presented suggest significant value in exploring innovative approaches to respiratory care that could address current gaps whilst positioning for future market leadership opportunities.

